Dry mouth, or xerostomia, is more than just a minor inconvenience—it can significantly affect daily life. When your salivary glands do not produce enough saliva, simple tasks like eating, speaking, and swallowing can become difficult. Additionally, dry mouth can lead to persistent bad breath, increased cavities, and gum disease.
While the condition can stem from various causes, from medications to lifestyle choices, the good news is that there are effective solutions. This guide will help you understand the causes, symptoms, and a wide range of treatments, from simple home remedies to medical interventions. Whether you experience occasional dryness or chronic discomfort, there is relief available, so keep reading for dry mouth treatments and solutions.
Table of Contents
What is Dry Mouth?
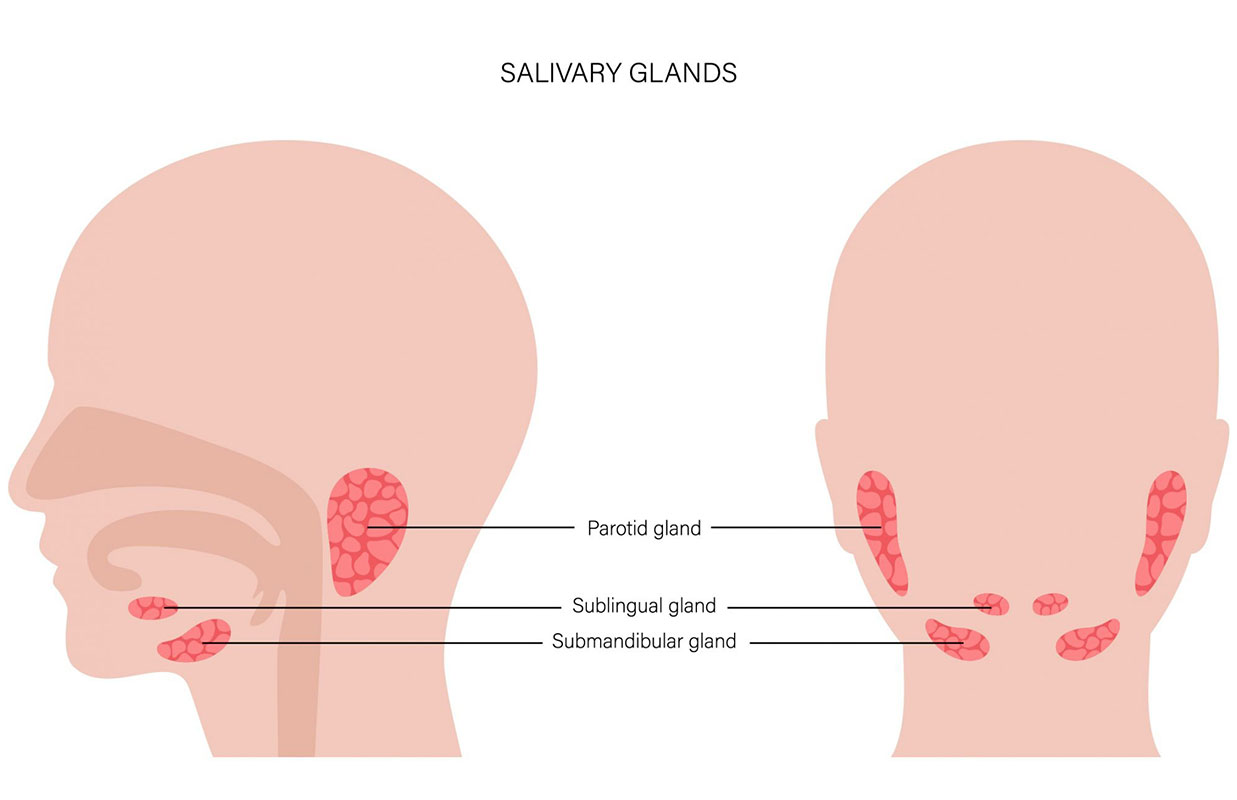
Before we get into dealing with dry mouth, let’s take a minute to understand what it is. Dry mouth, or xerostomia, is a condition where the salivary glands do not produce enough saliva to moisten the mouth. Saliva is crucial in digestion, oral health, and overall comfort. It helps break down food, neutralizes acids in the mouth, washes away food particles, and prevents bacterial growth. When saliva production is reduced, it can result in discomfort, difficulty eating and speaking, and an increased risk of dental problems such as cavities and gum disease. Dry mouth can be temporary or chronic, depending on the underlying cause. Identifying the cause of dry mouth is essential to implement the most effective treatment plan. Luckily, there are several effective dry mouth treatments and solutions to try.
Causes of Dry Mouth
Dry mouth can develop for various reasons, including lifestyle habits and underlying medical conditions. In some cases, it may be a temporary issue caused by dehydration or stress; in others, it may indicate a chronic problem requiring medical attention. Understanding the root cause of dry mouth is crucial for finding the most effective treatment. Below are some common factors that contribute to dry mouth:
Medications:
Many common prescription and over-the-counter medications list dry mouth as a side effect. These include antihistamines, decongestants, antidepressants, diuretics, muscle relaxants, and medications for high blood pressure. If you are on long-term medication, consult your doctor to determine if your prescriptions contribute to dry mouth.
Medical Conditions:
Certain chronic health conditions, such as diabetes, Sjögren’s syndrome, Parkinson’s disease, rheumatoid arthritis, lupus, and stroke, can interfere with saliva production. Autoimmune diseases, in particular, can directly target the salivary glands, reducing their ability to function properly.
Dehydration:
If you’re not drinking enough fluids, your body won’t produce enough saliva. Chronic dehydration can exacerbate dry mouth. Dehydration can result from illness, excessive sweating, fever, diarrhea, or inadequate fluid intake.
Mouth Breathing and Snoring:
Breathing through your mouth instead of your nose, especially while sleeping, can dry out oral tissues. Conditions like sleep apnea, nasal congestion, or deviated septum can contribute to mouth breathing and worsen dry mouth.
Cancer Treatments:
Radiation therapy to the head and neck and certain chemotherapy drugs can damage salivary glands, leading to chronic dry mouth. Radiation therapy in particular can permanently impair saliva production, making it crucial for cancer patients to seek specialized oral care.
Smoking and Alcohol Consumption:
Both smoking and excessive alcohol intake can decrease saliva production and worsen dry mouth symptoms. Smoking can also irritate oral tissues, while alcohol-based mouthwashes can dry out the mouth further.
Nerve Damage:
An injury or surgery affecting the head and neck area may impact the nerves responsible for saliva production. Nerve damage from trauma, surgery, or neurological conditions can disrupt normal saliva flow.
Aging:
Although dry mouth is not a direct result of aging, older adults are more likely to take multiple medications that can contribute to reduced saliva production. Additionally, certain age-related health conditions can lead to chronic dry mouth.
Nutritional Deficiencies:
A lack of essential nutrients, particularly vitamin A, vitamin B complex, and zinc, can affect saliva production. A balanced diet with sufficient vitamins and minerals is essential for maintaining healthy salivary glands.
Stress and Anxiety:
High levels of stress and anxiety can lead to temporary dry mouth due to the body’s natural fight-or-flight response. Chronic stress can also lead to lifestyle habits, such as drinking less water or consuming more caffeine, exacerbating dry mouth.
Symptoms of Dry Mouth

Experiencing dry mouth can lead to a variety of symptoms that impact oral health, digestion, and overall well-being. Some symptoms are mild and temporary, while others may persist and require medical intervention. The severity of symptoms often depends on the underlying cause and how long the condition has been present. Recognizing these symptoms early can help you take steps to alleviate discomfort and prevent further complications. Below are the most common signs of dry mouth:
Persistent Dryness or Stickiness
One of the most noticeable symptoms is a constant dry, parched feeling in the mouth, throat, and even the lips.
Difficulty Chewing, Swallowing, or Speaking:
Saliva plays a crucial role in breaking down food and aiding speech. Without enough moisture, you might struggle to chew correctly, swallow food comfortably, or even speak without feeling hoarse.
A Rough, Dry, or Grooved Tongue:
Due to a lack of moisture, your tongue might feel rough, appear cracked, or develop grooves. This can also make eating spicy or acidic foods uncomfortable.
Frequent Thirst:
Even after drinking water, you may still feel thirsty due to a lack of sustained saliva production.
Cracked Lips and Mouth Sores:
The absence of saliva can make your lips dry, cracked, or prone to peeling. Some people also develop painful sores or ulcers inside their mouths.
Burning or Tingling Sensation in the Mouth:
A persistent burning or tingling feeling on your tongue or inner cheeks, also known as burning mouth syndrome, can occur with dry mouth.
Increased Occurrences of Bad Breath:
Saliva helps cleanse your mouth of bacteria and food particles. When production is low, bacteria thrive, leading to chronic bad breath.
Higher Susceptibility to Cavities and Gum Disease:
Without adequate saliva to neutralize acids and wash away food debris, bacteria can rapidly multiply, increasing your risk of cavities, gum inflammation, and periodontal disease.
Altered Taste Sensation:
Some people with dry mouth experience a diminished sense of taste or a persistent metallic or bitter taste in their mouth.
Hoarseness and Dry Throat:
A dry mouth often leads to a dry throat, which can result in hoarseness, sore throat, and difficulty speaking for long periods
Home Remedies for Dry Mouth

If you’re looking for natural and effective ways to manage dry mouth, several home remedies can provide relief. Many of these remedies focus on increasing moisture in the mouth, stimulating saliva production, and avoiding irritants that may worsen symptoms. Simple changes to your daily routine, diet, and oral hygiene habits can significantly alleviate discomfort. Below are some of the most effective home remedies for dry mouth:
Stay Hydrated:
Drinking plenty of water throughout the day is essential to moisten your mouth. Aim for small, frequent sips rather than large amounts at once. Herbal teas and cucumber or lemon-infused water can also help keep your mouth fresh.
Chew Sugar-Free Gum or Lozenges:
Sugar-free gum and lozenges stimulate saliva production, providing immediate relief. Look for options containing xylitol, as it not only promotes moisture but also helps prevent cavities.
Avoid Caffeine and Alcohol:
Caffeinated drinks like coffee and sodas can dehydrate your mouth, worsening dryness. Alcohol, including alcohol-based mouthwashes, can also dry out oral tissues. Instead, opt for non-caffeinated herbal teas and alcohol-free mouth rinses.
Use a Humidifier:
Sleeping with a humidifier in your bedroom can add moisture to the air and prevent your mouth from drying out overnight.
Practice Good Oral Hygiene:
Brush your teeth at least twice daily with fluoride toothpaste and use an alcohol-free mouthwash. Floss regularly to remove food particles that could contribute to bacterial growth in a dry mouth environment.
Eat Moisture-Rich Foods:
To help maintain oral moisture levels, consume foods with high water content, such as watermelon, celery, apples, cucumbers, and yogurt.
Limit Sugary and Salty Foods:
Excess sugar and salt can contribute to dehydration and increase bacteria in the mouth, leading to worsened symptoms.
Try Coconut or Olive Oil Pulling:
Swishing a tablespoon of coconut or olive oil in your mouth for a few minutes daily can provide a protective coating and retain moisture.
Use Aloe Vera Gel:
Applying aloe vera gel to the inside of your mouth can soothe dryness and help retain moisture naturally.
Suck on Ice Chips:
Slowly sucking on ice chips can provide instant relief and help stimulate saliva flow.
Over-the-Counter Products for Dry Mouth Relief

If home remedies are not providing enough relief, there are several over-the-counter (OTC) products available to help combat dry mouth:
Artificial Saliva Substitutes:
These mimic natural saliva and provide moisture to the mouth. Products such as Biotene Oral Balance Gel and Oasis Moisturizing Mouth Spray are designed to relieve dryness and discomfort.
Mouthwashes for Dry Mouth:
Alcohol-free mouthwashes like Biotene Dry Mouth Oral Rinse or ACT Dry Mouth Mouthwash help hydrate the mouth and freshen breath without irritating sensitive tissues.
Moisturizing Lozenges and Gels:
Products such as XyliMelts, TheraBreath Dry Mouth Lozenges, and Oracoat Dry Mouth Discs dissolve slowly in the mouth to provide extended relief and stimulate saliva production.
Xylitol-Based Products:
Chewing gum and mints containing xylitol help stimulate saliva flow and reduce the risk of cavities by inhibiting bacterial growth in the mouth.
Dry Mouth Sprays:
Sprays like Salivart and Mouth Kote provide quick relief and can be used as needed throughout the day.
Hydrating Toothpastes:
Fluoride-rich, dry-mouth-friendly toothpaste such as Biotene Fluoride Toothpaste or Colgate Hydris help protect teeth and gums while keeping the mouth moist.
Humectant-Based Lip Balms:
Dry lips can accompany dry mouth, and using lip balms with natural humectants like aloe vera or beeswax can help keep lips hydrated and prevent cracking.
Regularly using these products can relieve and help manage dry mouth symptoms effectively. Combining OTC treatments with proper oral hygiene and hydration can significantly affect comfort and oral health.
Medical Treatments for Chronic Dry Mouth

Medical treatments may be necessary if dry mouth persists despite home remedies and over-the-counter solutions. These treatments aim to stimulate saliva production or manage underlying conditions causing dryness:
Prescription Medications:
Drugs like pilocarpine (Salagen) and cevimeline (Evoxac) are often prescribed to stimulate saliva production in individuals with chronic dry mouth, especially those with conditions like Sjögren’s syndrome.
Salivary Gland Stimulation Therapy:
This includes electrostimulation devices that gently stimulate the salivary glands to produce more saliva. These treatments are often recommended for individuals who have suffered nerve damage or undergone radiation therapy.
Botox Injections:
In cases where overactive salivary gland function is an issue, Botox injections may be used to regulate saliva flow and prevent extreme dryness.
Treatment of Underlying Conditions:
If an existing medical condition is contributing to dry mouth, managing the primary issue—such as optimizing diabetes control or treating autoimmune diseases—can help alleviate symptoms.
Medication Adjustments:
If a prescription drug is causing dry mouth, a healthcare provider may modify the dosage or suggest an alternative medication with fewer drying effects.
Surgical Procedures:
In rare cases, surgical interventions such as salivary gland transplants may be considered for individuals with severe, irreversible dry mouth due to glandular damage.
Hydration Therapy:
In severe cases of dehydration-related dry mouth, intravenous (IV) fluids may be administered to restore hydration levels and support normal salivary function.
For individuals experiencing persistent and severe dry mouth, consulting a healthcare professional is essential to determine the most effective course of treatment.
How Your Dentist Can Help

Your dentist plays a crucial role in diagnosing, managing, and treating dry mouth. They can help identify whether medications, an underlying health condition, or lifestyle factors cause your condition. Dentists can also recommend specialized oral care products, such as prescription-strength fluoride toothpaste, mouth rinses, or saliva substitutes tailored to your needs. Additionally, they offer preventive treatments like fluoride applications and regular cleanings to reduce the risk of cavities and gum disease, which can be exacerbated by dry mouth.
If saliva production is insufficient, your dentist may suggest saliva stimulation strategies, including xylitol-based gums or lozenges. For severe cases, they may collaborate with other healthcare professionals to create a customized treatment plan, which could involve medication adjustments or lifestyle modifications. If you wear dentures, your dentist can provide solutions to prevent irritation and improve comfort in a dry mouth environment. Regular dental visits and open communication with your dentist are essential for effectively managing dry mouth and maintaining optimal oral health.
In Conclusion
Saliva is very important to your oral well-being, and living with dry mouth can be frustrating, but there are many ways to find relief. You can significantly improve your comfort and oral health by staying hydrated, adjusting your diet, using saliva-stimulating products, and addressing any underlying conditions. If symptoms persist despite trying home remedies and OTC treatments, consult a healthcare professional to explore medical options. You don’t have to suffer in silence—help is available, and a well-moisturized mouth can make a world of difference in your daily life!
It depends on the cause. If dry mouth is due to medication or a chronic condition, managing the underlying issue can help, but some cases require long-term management.
Yes, dry mouth is more common in older adults because of age-related health conditions and medications that reduce saliva production.
High levels of stress and anxiety can trigger dry mouth by reducing saliva production as part of the body’s fight-or-flight response.
Yes, dry mouth can make it uncomfortable to breathe, increase snoring, and lead to frequent waking due to thirst.
Yes, your dentist can recommend treatments, prescribe fluoride toothpaste or mouth rinses, and monitor for oral health issues caused by dry mouth.
No, dry mouth itself is not contagious. However, some underlying causes, such as infections, may be transmissible.
Check us out on Facebook and Twitter for daily information about Oral Health from Martindale Dental, or visit our offices in Hamilton and St. Catharines.
Have more questions?
Please contact us for all inquiries or to book an appointment with one of our convenient clinic locations. We look forward to hearing from you.




