Root Canal
Cavities, damaged teeth and facial trauma can allow bacteria to enter the pulp of a tooth and cause an infection. If this happens, a root canal procedure is required to save the affected tooth. This procedure removes the infected pulp and seals the tooth to prevent bacteria from entering and causing another infection.
Table of Contents
Overview
What is a root canal procedure?
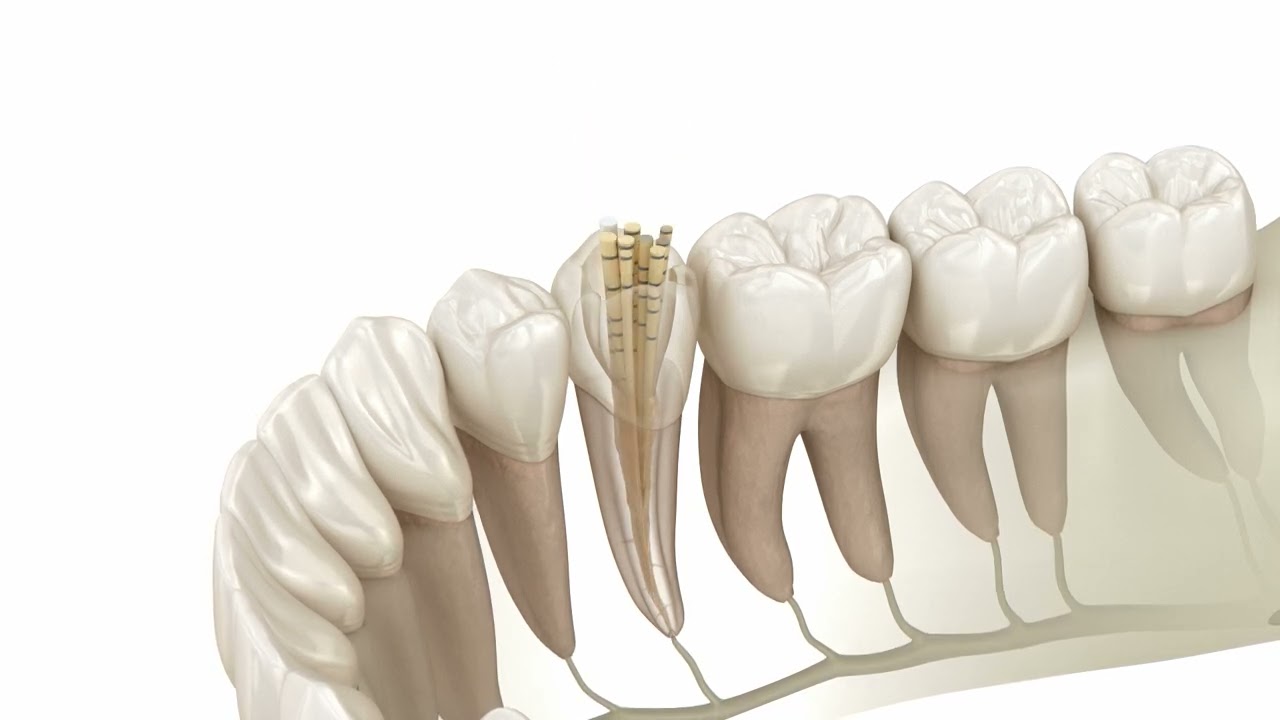
A root canal is a dental procedure that involves removing the pulp (the soft inner tissue) from the inside of a tooth when it becomes infected, inflamed, or damaged (abscessed tooth). The pulp contains nerves, blood vessels, and connective tissue. When it gets infected, it can cause severe pain, sensitivity to hot and cold temperatures, swelling, and even abscess formation.
How common are root canal procedures?
Root canals are relatively common dental procedures. While the thought of a root canal might evoke concerns due to its reputation for being painful, modern dental techniques and anesthetics have significantly improved the experience for patients.
What does a root canal procedure do?
Root canals are often recommended to preserve a tooth’s functionality and appearance rather than opting for extraction. Losing a tooth can lead to issues like difficulty chewing, shifting of surrounding teeth, and potential bone loss in the jaw. Our dental team always tries to preserve your natural teeth if at all possible.
When is a root canal necessary?
A root canal procedure is necessary when the pulp of a tooth becomes infected, inflamed, or damaged. The most common reason for this to happen is when a cavity is left untreated, but this can occur due to various reasons, including:
Dental decay
If a cavity is left untreated, it can eventually reach the inner pulp of the tooth, leading to infection and inflammation.
Dental trauma
Even if there is no visible damage, a tooth that has suffered a significant impact or injury can damage the pulp.
Deep fillings
Large and deep dental fillings can sometimes irritate the pulp, leading to inflammation and infection.
Cracked or fractured tooth
A crack or fracture in a tooth can allow bacteria to enter the pulp, causing infection and inflammation.
Repeated dental procedures
Multiple dental procedures on the same tooth, such as fillings or crowns, can weaken the tooth’s structure and increase the risk of pulp damage.
Gum disease
Advanced gum disease can lead to the exposure of the tooth’s roots, making them susceptible to infection.
Abscess
If an infection within the pulp is left untreated, it can spread to the root tip and form a pus-filled pocket called an abscess.
What are the symptoms that a root canal is required?
The symptoms of a tooth that might require a root canal can vary, but they often involve pain, sensitivity, and changes in the tooth’s appearance or surrounding tissues. Some common symptoms include:
Severe and lasting toothache
Intense, throbbing, or continuous pain in the tooth is one of the most common symptoms. The pain might increase when you bite down or apply pressure to the tooth. The pain won’t go away over time.
Sensitivity to temperature
Increased sensitivity to hot or cold temperatures, even after the temperature stimulus is removed, can signal pulp inflammation or infection.
Painful chewing
Discomfort or pain when chewing or biting down on the affected tooth can indicate pulp or nerve involvement.
Swelling
Swelling of the gums around the affected tooth can occur, often accompanied by tenderness and a possible pimple-like bump called a gum abscess.
A cracked or chipped tooth
A damaged tooth can allow bacteria to get into the pulp of the tooth, which will ultimately require a root canal to repair.
A loose tooth
An infected tooth will typically feel loser as pus from the infection softens the bone which is supporting the tooth.
Discoloration
The affected tooth might appear darker or grayer than the surrounding teeth, indicating internal damage or infection.
Gum pimples
If you notice a boil or pimple has developed on your gums near a painful tooth, with or without pus drainage, it could be a sign that you have an abscessed tooth which requires a root canal.
Prolonged pain
Pain that lingers after exposure to hot or cold substances or pain that wakes you up at night can be indicative of an underlying issue.
Bad taste or odour
An unpleasant taste in the mouth or a foul odour might develop if an infection or abscess is associated with the affected tooth.
Radiating pain
Pain might radiate to the jaw, ear, or other nearby areas if the infection or inflammation has spread.
General discomfort
A general feeling of unease or discomfort in the area around the affected tooth can indicate an underlying problem.
It’s important to note that not all cases of tooth pain or discomfort require a root canal. However, if you are experiencing any of these symptoms, scheduling an appointment with a dentist as soon as possible is recommended. They can perform a thorough examination, possibly including X-rays, to determine the underlying issue and recommend appropriate treatment, which might include a root canal if necessary. Early intervention can help prevent further complications and preserve the tooth’s health.
About the procedure
What happens during a root canal procedure?
A root canal procedure involves several steps and is typically performed by a dentist or an endodontist (a dentist that specializes in root canal treatments). Here’s an overview of what happens during a root canal procedure:
- Diagnosis
Before the procedure, the dentist will examine the tooth and may take X-rays to assess the extent of the damage to the pulp and the surrounding structures.
- Anesthesia
The tooth and the surrounding area will be numbed with a local anesthetic to ensure that you are comfortable and don’t feel any pain during the procedure.
- Isolation dam
A rubber dam or other protective barrier is placed around the tooth to keep it dry and prevent saliva contamination.
- Access opening
The dentist creates a small opening in the tooth’s crown to access the pulp chamber and root canals.
- Pulp removal
The infected or damaged pulp tissue is carefully removed from the pulp chamber and root canals using specialized instruments. The inside of the tooth is then cleaned and disinfected to remove any bacteria and debris.
- Shaping and irrigation
The dentist shapes the root canals to prepare them for filling. This helps ensure that the canals are thoroughly cleaned and ready for sealing. Irrigation solutions are used to flush out any remaining debris and disinfect the canals.
- Filling
Once the canals are cleaned and shaped, they are filled with a biocompatible gutta-percha material. This material seals the canals and prevents future infection.
- Sealing
The access opening created at the beginning of the procedure is sealed with a temporary or permanent filling. In some cases, a dental crown may be recommended to provide additional protection and strength to the tooth.
- Restoration placement
If a dental crown is not placed immediately after the root canal, the dentist might recommend scheduling a follow-up appointment to place a crown. This is especially common for back teeth, which endure more chewing force.
How long does a root canal take?
The duration of a root canal procedure can vary depending on several factors, including the complexity of the tooth’s anatomy, the severity of the infection or damage, and the dentist’s experience. On average, a straightforward single-rooted tooth root canal procedure can be completed in one appointment and will take 30 to 60 minutes. However, a more complex procedure involving multiple roots or complications might require additional appointments.
Are root canals painful?
Modern root canal procedures are typically less painful than their reputation suggests. With the use of local anesthesia and advancements in dental techniques, most patients report minimal to no pain during the procedure. Once the infection is removed, most patients feel immediate relief once the procedure is completed. Some minor discomfort or mild soreness might be experienced after the procedure once the anesthesia wears off. Still, this discomfort is often manageable with over-the-counter pain relievers and usually subsides within a few days.
Swelling or severe throbbing pain is not normal after treatment, and you should get in touch with your dentist immediately.
How to prepare for a root canal procedure
Preparing for a root canal procedure involves a combination of understanding the process, communicating with your dentist, and making arrangements to ensure your comfort and well-being. Here’s a guide on how to prepare for a root canal procedure:
Consultation
Schedule a consultation with your dentist to discuss the procedure, ask questions, and address any concerns you might have. Inform your dentist about any allergies, medications you’re taking, or health conditions.
Follow instructions and take medications
Follow any pre-procedure instructions provided by your dentist. This might include fasting if you’ll be receiving sedation. If you’re prescribed antibiotics before the procedure, take them as directed to control any existing infection.
Arrange transportation
If sedation or anesthesia is used during the procedure, arrange for someone to drive you to and from the dental office, as you might not be fit to drive immediately after the procedure.
Eat lightly
If you’re not required to fast, opt for a light meal before the procedure to help you feel comfortable. Avoid heavy or overly spicy foods.
Comfort items
Bring headphones, music, or an audiobook to help you relax during the procedure. Wear comfortable clothing and bring a light sweater or blanket to stay warm.
Plan for aftercare
Prepare soft foods and cold drinks to consume after the procedure while you may experience some soreness. Arrange for time off work or other activities if needed, especially if you anticipate needing some rest after the procedure.
Benefits & Risks
Benefits of a root canal procedure
Opting for root canal therapy offers several advantages, including the ability to:
- Stop the spread of infection to neighbouring teeth.
- Alleviate symptoms linked to an abscessed tooth.
- Minimize the likelihood of jawbone damage.
- Avoid tooth extraction.
- Avoid damage to your jawbone which could require a bone grafting procedure to repair.
Are root canal procedures safe?
Modern root canal treatments are considered to be safe, with a 98% success rate. While a root canal is not recommended for women in their first or third trimester of pregnancy, your dentist may be able to perform the procedure during the second trimester, provided only a local anesthetic is required.
What happens if a root canal fails?
Failed root canals are rare, but if it does happen, your dentist may perform another root canal as soon as possible or discuss alternative treatment options.
Symptoms of a failed root canal procedure?
In isolated cases, root canal complications can occur. This is usually only when a tooth is too damaged for a root canal procedure to be effective. The symptoms of a failed root canal include:
- Pain that doesn’t go away
- Draining pus from the affected area
- Visible pimple or boil
- Tooth discolouration
- Swollen gums
- Sinus problems
Root canal alternatives
While there aren’t any direct alternatives to a root canal, some tooth infections can be treated successfully with antibiotics. Otherwise, a tooth extraction will be required to maintain your oral health.
If you’re not a candidate for a root canal procedure, the affected tooth can be extracted, and a dental implant, bridge or partial denture can be installed.
Recovering from a root canal
How long does it take to recover after a root canal treatment?
In most cases, the recovery time after a root canal is less than a week. While many patients report immediate relief, some patients may experience mild discomfort for a few days, which can be managed with pain relief medication.
If you have lasting or severe pain, contact our office immediately.
Can I drive home after a root canal?
The answer depends on the type of anesthesia you had during the procedure. If only a local anesthetic or nitrous oxide gas was used, you could drive after treatment. Some patients opt for IV or oral sedation, in which case operating a motor vehicle after the root canal is not recommended.
Will I be able to eat after a root canal?
While you can eat immediately after a root canal, it’s best to wait until the effects of the anesthetic have worn off before eating.
Regarding what you can eat, it’s recommended to choose softer foods – yogurt, pasta, mashed potatoes, smoothies – for a day or two until any lingering tooth pain disappears. You should not bite or chew using the treated tooth for a few days or until a dental restoration has been installed. Check out our article on foods to eat after wisdom tooth surgery for some more tips.
Root canal aftercare
The most important aspect of root canal aftercare is to keep the area clean. This means brushing and flossing as usual, and adding an antibacterial mouthwash to your routine. A properly performed root canal should last a lifetime unless other complications or dental health issues arise.
Martindale Dental provides both general and specialty dentistry under one roof. For more than 20 years, our dentists have been advocates for their patient’s oral health care needs.
Our dental offices are conveniently located throughout the GTA in Hamilton (Jackson Square), and St. Catharines, Ontario. We offer convenient appointments before or after work & on weekends.
Martindale Dental provides both general and specialty dentistry under one roof. For more than 20 years, our dentists have been advocates for their patient’s oral health care needs.
Our dental offices are conveniently located throughout the GTA in Hamilton (Jackson Square), and St. Catharines, Ontario. We offer convenient appointments before or after work & on weekends.
