Ever wondered if your mouth is trying to tell you something? Bad dental hygiene doesn’t just lead to cavities—it can signal deeper health issues. From bad breath to bleeding gums, your oral health reflects your overall well-being. Recognizing the signs of poor dental hygiene early can prevent serious complications down the line.
In this article, we’ll explore the top 10 signs of bad dental hygiene, delve into their causes, and provide actionable tips to enhance your oral health. Understanding these signs is crucial for maintaining a healthy smile and body, whether you’re a teenager, adult, or senior.
Table of Contents

1. Persistent Bad Breath (Halitosis)
Bad breath might seem like a minor annoyance — something a mint or a quick swish of mouthwash can fix. But when it’s chronic, it’s usually a sign that something more serious is going on inside your mouth. Known as halitosis, persistent bad breath is often caused by bacteria thriving in leftover food particles, plaque, or even infections. It’s not just a social embarrassment; it could be your mouth’s way of alerting you to deeper issues with your oral hygiene or overall health.
Causes:
- Poor oral hygiene: Inadequate brushing and flossing allow food particles to remain in the mouth, promoting bacterial growth between teeth, around the gums, and on the tongue. This bacterial accumulation produces sulphur compounds, leading to unpleasant odours.
- Dry mouth (xerostomia): Saliva helps cleanse the mouth by neutralizing acids produced by plaque and washing away dead cells. Reduced saliva production can lead to bad breath.
- Diet: Certain foods, such as onions, garlic, and spices, can cause bad breath. After digestion, their breakdown products are carried in the blood to the lungs, affecting the breath.
Tobacco products: Smoking or chewing tobacco not only introduces odorous chemicals into the mouth but also dries out the oral cavity and damages gum tissues, all of which contribute to lingering bad breath. - Medical conditions: Certain systemic diseases like diabetes, sinus infections, acid reflux, and kidney or liver disorders can manifest as chronic bad breath due to imbalances in bodily chemistry or increased bacterial presence.
Treatment Options:
- Maintain good oral hygiene: Brushing at least twice a day and flossing daily removes plaque and food debris. Using a tongue scraper can also help eliminate accumulated bacteria on the tongue.
- Stay hydrated: Drinking water regularly helps rinse the mouth and promotes saliva production, both of which are essential for controlling bacteria levels.
- Use mouthwash: These can reduce the bacterial load in your mouth and temporarily mask odours. Look for those containing chlorhexidine or cetylpyridinium chloride.
- Regular dental check-ups: Regular professional cleanings help eliminate tartar and detect any dental issues early, like gum disease or cavities, that might be causing bad breath.
- Address underlying conditions: If oral hygiene doesn’t improve breath, a physician can evaluate for other conditions that might be the root cause.

2. Bleeding Gums
A little blood in the sink after brushing might seem harmless, but gums aren’t supposed to bleed — not even a little. Bleeding gums are among the earliest and most common warning signs of gum disease. Often caused by plaque buildup along the gumline, bleeding is your body’s inflammatory response to bacterial irritation. Left untreated, it can develop into something far more serious, including gum recession and even tooth loss.
Causes:
- Gingivitis: This is the earliest stage of gum disease, marked by inflammation and bleeding, especially when brushing or flossing. It results from plaque buildup along the gumline, which triggers an immune response, causing the gums to swell and bleed.
- Improper brushing or flossing: Brushing too hard or snapping floss between teeth can cause physical trauma to gum tissues, leading to irritation and bleeding. A soft-bristled brush and gentle technique are key.
- Vitamin deficiencies: A lack of vitamin C can weaken the gums’ blood vessels and connective tissue, making them more prone to bleeding. Vitamin K deficiency can impair blood clotting.
- Hormonal changes: During pregnancy, menstruation, or menopause, hormonal fluctuations can increase blood flow to the gums, making them more sensitive and susceptible to bleeding.
- Medical conditions: Bleeding disorders (like hemophilia), leukemia, or uncontrolled diabetes can manifest as gum bleeding. Medications like blood thinners can also play a role.
Treatment Options:
- Improve oral care routine: Switch to a soft-bristled brush and use correct flossing techniques. Rinse with an antiseptic mouthwash to reduce inflammation and bacteria.
- Professional Cleaning: A dentist can perform scaling and root planing to remove plaque and tartar beneath the gumline.
- Nutritional Support: Incorporate vitamin-rich foods or supplements to address deficiencies.
- Monitor Hormonal Fluctuations: Consult with a healthcare provider to manage gum sensitivity during hormonal shifts.
- Medical Evaluation: Persistent bleeding should be evaluated by a dentist or doctor to rule out underlying systemic conditions.

3. Tooth Sensitivity
If sipping hot coffee or biting into an ice cream cone sends a jolt of pain through your teeth, you’re not alone — and it’s not normal. Tooth sensitivity occurs when the protective enamel wears down or when gums recede, exposing the inner layers of your teeth. These inner parts contain tiny nerve endings that react strongly to temperature changes, sweets, or even brushing. While it may start as a mild annoyance, it often points to underlying issues like enamel erosion or gum disease that need to be addressed.
Causes:
- Enamel Erosion: Acidic foods, beverages (like soda or citrus juice), and aggressive brushing can wear down the protective enamel layer. Without enamel, the dentin underneath becomes exposed, leading to discomfort when eating or drinking.
- Gum Recession: Often due to gum disease or brushing too hard, this condition exposes the sensitive root surfaces of teeth that lack enamel protection, making them highly reactive to temperature changes.
- Tooth Decay or Cavities: When decay penetrates enamel and reaches the dentin or pulp, it irritates the nerves inside the tooth, leading to sharp pain when stimulated.
- Cracked or Fractured Teeth: A crack allows external stimuli—like cold air or sweet foods—to reach the inner tooth layers, causing pain.
- Bruxism: Grinding your teeth wears down enamel over time, exposing the underlying dentin and creating sensitivity.
Treatment Options:
- Desensitizing Toothpaste: These products contain potassium nitrate or stannous fluoride to help block pain signals from the tooth surface to the nerve.
- In-Office Fluoride Treatments: Fluoride strengthens enamel and reduces transmission of pain signals.
- Bonding or Sealants: Dentists can apply a tooth-colored resin to cover exposed roots and prevent sensitivity.
- Night Guards: Custom-fitted guards prevent enamel damage caused by nighttime grinding.
- Dietary Adjustments: Reducing intake of acidic or overly sweet foods helps protect enamel from erosion.

4. Visible Plaque and Tartar
Plaque is a soft, sticky film of bacteria that forms on your teeth throughout the day, and if you don’t remove it regularly, it can harden into tartar, a yellowish or brown deposit that clings stubbornly to your enamel. While it might seem like just a cosmetic issue, tartar is a serious threat to your oral health. It acts like a bacteria magnet, leading to gum inflammation, bad breath, and eventually cavities and gum disease. If you’re seeing or feeling tartar buildup, it’s a clear sign your oral hygiene habits need some tweaking.
Causes:
- Poor Oral Hygiene: Plaque is a sticky, colourless film of bacteria that constantly forms on your teeth. If you don’t brush and floss properly and regularly, plaque builds up and eventually hardens into tartar, a crusty deposit that can only be removed by a dental professional. Tartar makes it easier for more plaque to adhere, setting off a vicious cycle.
- Diet High in Sugars and Starches: Sugary and starchy foods feed the bacteria in plaque, accelerating its formation. These bacteria produce acids that not only help plaque grow but also erode tooth enamel over time.
- Dry Mouth: Saliva is critical in neutralizing acids and washing away food particles. A dry mouth (due to medications, health conditions, or dehydration) means bacteria and plaque are more likely to accumulate unchecked.
Treatment Options:
- Brush and Floss Consistently: Brushing twice daily and flossing once a day helps remove plaque before it hardens into tartar. Use a fluoride toothpaste and pay close attention to the gumline.
- Professional Dental Cleaning: Once tartar forms, brushing alone is insufficient. A hygienist or dentist uses special tools to remove tartar from teeth during routine cleanings.
- Antibacterial Mouthwash: Rinsing with a mouthwash that targets plaque-forming bacteria can offer extra protection between brushing.
- Healthy Diet: Reducing intake of sugary snacks and acidic beverages helps starve the bacteria that cause plaque.
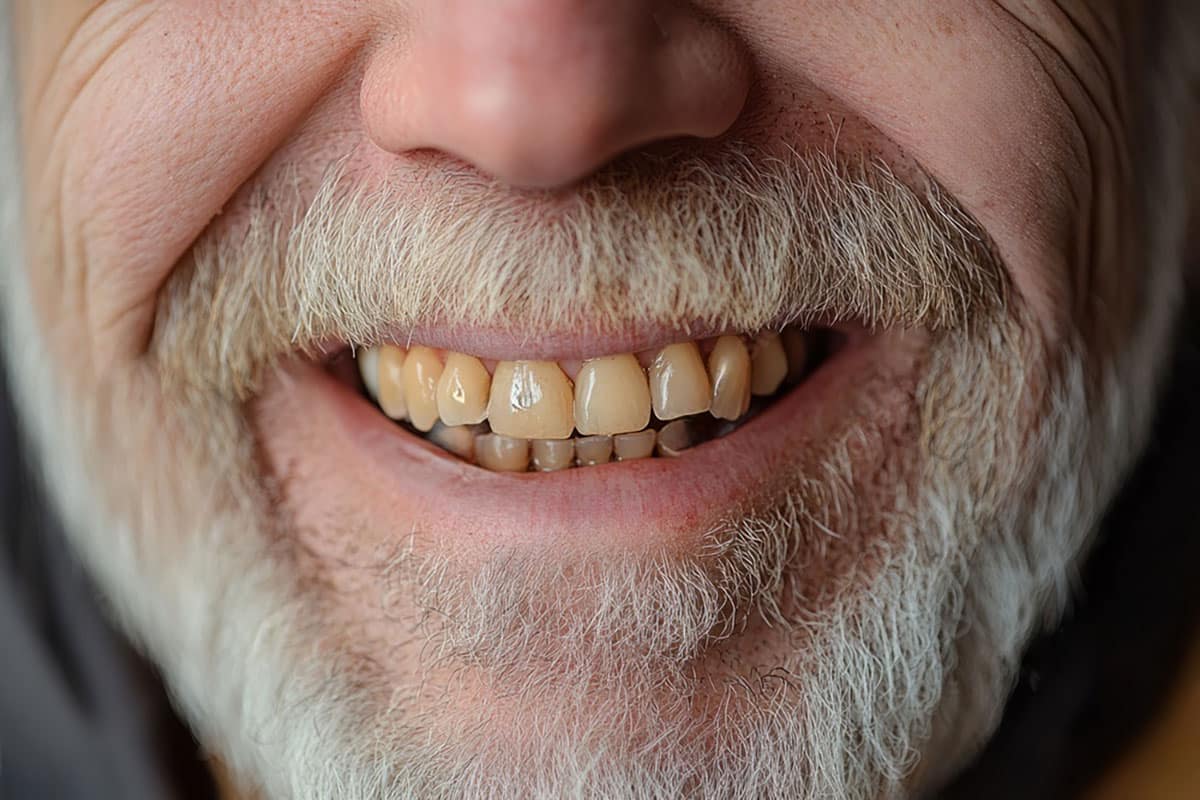
5. Discoloured or Stained Teeth
We all want a bright, confident smile, but it can be discouraging when teeth start turning yellow, brown, or dull gray. While discoloration is often dismissed as a cosmetic concern, it can also reflect deeper oral hygiene issues or lifestyle habits. Stains can be caused by foods, drinks, tobacco, or even medications, but plaque buildup and enamel erosion can amplify the effect. The appearance of your teeth reflects your oral habits, and a warning sign if something’s off.
Causes:
- Foods and Beverages: Drinks like coffee, tea, cola, and red wine contain chromogens—intensely pigmented molecules that bind to enamel and cause staining. Berries and tomato sauces have similar effects.
- Tobacco Use: Nicotine and tar in tobacco products penetrate the pores in your enamel and cause stubborn yellow or brown stains.
- Poor Oral Hygiene: If you’re not brushing or flossing thoroughly, plaque and food stains can stick around longer, compounding the discoloration over time.
- Aging: As you age, enamel wears down, making the yellowish dentin layer beneath more visible. This natural process can make your teeth appear darker or duller.
- Medications or Fluorosis: Certain antibiotics (like tetracycline) taken in childhood or excess fluoride can affect the development or colour of enamel, leading to intrinsic stains.
Treatment Options:
- Whitening Toothpaste or Kits: For surface stains, whitening toothpaste or over-the-counter kits may help. These are often effective for coffee and food stains, but not for deeper discoloration.
- Professional Whitening Treatments: In-office bleaching uses stronger agents that penetrate enamel and can significantly whiten teeth in one or more visits.
- Veneers or Bonding: For internal discoloration that doesn’t respond to whitening, dental veneers or composite bonding can cover stained teeth and restore a white appearance.
- Lifestyle Changes: Cutting back on staining foods and drinks—and quitting smoking—can prevent future discoloration.

6. Receding Gums
Gums are vital in anchoring and protecting your teeth, but they’re also surprisingly delicate. It’s known as gum recession when it starts pulling back from the tooth surface, exposing roots and creating gaps. It’s not just about appearance; gum recession increases your risk of sensitivity, decay, and tooth loss. While it can be caused by aggressive brushing, it’s more often a red flag for progressing gum disease.
Causes:
- Gum Disease (Periodontitis): When plaque and tartar aren’t removed, they can cause gums to become inflamed and pull away from the teeth. As periodontitis progresses, it destroys supporting bone and tissue, making gum recession worse.
- Aggressive Brushing: Brushing too hard or using a hard-bristled toothbrush can wear away gum tissue over time, especially along the gumline.
- Poor Dental Habits: Infrequent flossing, skipping cleanings, or ignoring early signs of gum inflammation can lead to long-term damage.
- Tobacco Use: Smoking reduces blood flow to the gums, slowing healing and promoting gum detachment.
- Genetics or Misaligned Teeth: Some people are genetically predisposed to thinner gum tissue or may experience recession due to bite issues or tooth grinding.
Treatment Options:
- Improved Brushing Technique: Use a soft-bristled toothbrush and gentle circular motions. Avoid back-and-forth scrubbing that can damage tissue.
- Scaling and Root Planing: This deep cleaning procedure removes plaque/tartar from below the gumline and smooths root surfaces to help gums reattach.
- Gum Grafts or Pinhole Surgery: In cases of severe recession, a periodontist may perform a graft using your own tissue or a donor source to restore the gumline.
- Address Underlying Causes: Treat bruxism with a night guard, quit smoking, and fix bite alignment if needed.

7. Loose or Shifting Teeth
Your adult teeth are supposed to be permanent, so something is wrong if one feels even slightly loose. Loose or shifting teeth can indicate serious structural problems beneath the surface, often due to advanced periodontal disease weakening the bone and tissue that support your teeth. Sometimes, it’s caused by trauma or chronic grinding. Either way, this is one of the more urgent dental signs that shouldn’t be ignored.
Causes:
- Advanced Gum Disease (Periodontitis): When plaque and tartar are left to build up along the gumline, they cause inflammation that destroys the tissues holding your teeth in place. As periodontitis progresses, the bone that supports your teeth starts to break down, leading to teeth that feel wobbly or begin to shift positions, often one of the most serious signs of oral neglect.
- Trauma or Physical Injury: An accidental hit to the mouth — from a fall, sports injury, or even biting down too hard — can dislodge a tooth from its socket or damage the ligaments that anchor it. If the tooth isn’t stabilized quickly, it can become permanently loose or misaligned.
- Bruxism (Teeth Grinding): Chronic grinding or clenching puts excessive, uneven pressure on your teeth. Over time, this force wears away the structures supporting your teeth, which can lead to mobility, especially in the back molars or front teeth.
- Bone Loss (Osteoporosis or Other Conditions): Your teeth rely on a healthy jawbone for support. Systemic bone-thinning diseases like osteoporosis, or even long-term untreated periodontitis, can reduce bone density in the jaw, loosening teeth over time.
Treatment Options:
- Periodontal Therapy: If gum disease is the cause, deep cleanings like scaling and root planing are the first line of defence. These remove plaque and tartar below the gumline and smooth root surfaces to help gums reattach to teeth.
- Splinting Loose Teeth: A dentist may “splint” a mobile tooth by bonding it to neighbouring teeth, stabilizing it while healing occurs. This is often done using composite resin or a small wire on the back of the teeth.
- Custom Mouthguards (for Bruxism): A night guard helps prevent damage from grinding while you sleep. It cushions the pressure and preserves tooth structure and alignment.
- Surgical Intervention or Bone Grafts: In severe cases, periodontists may use bone grafts to regenerate lost bone tissue or recommend surgeries to reposition and stabilize the teeth.
- Tooth Replacement: If a tooth can’t be saved, options like dental implants, bridges, or partial dentures restore both function and aesthetics.

8. Mouth Sores or Ulcers
A canker sore here or there might not be alarming, but frequent sores inside your mouth can signal more than just irritation. Sores, ulcers, or white patches might result from simple things like a sharp chip or spicy food, but they can also be a sign of infections, immune responses, or nutritional deficiencies. Paying attention to these small but painful spots can help you detect larger health issues early.
Causes:
- Physical Trauma: Accidentally biting your cheek, rubbing from poorly fitted dentures, or irritation from braces or dental appliances are all common triggers for oral sores. Even sharp or jagged teeth can scrape the inside of your mouth, leading to ulcers.
- Canker Sores (Aphthous Ulcers): These are non-contagious, small white or yellowish ulcers with a red border. They’re often linked to stress, fatigue, hormonal changes, acidic foods, or minor injuries. While not dangerous, they can be painful, especially when eating or speaking.
- Viral Infections (Herpes Simplex): Cold sores are caused by the herpes simplex virus (HSV-1). These painful, fluid-filled blisters appear around the lips or inside the mouth and are highly contagious. Outbreaks can be triggered by stress, illness, or sun exposure.
- Fungal Infections (Oral Thrush): A yeast infection in the mouth (usually caused by Candida albicans) appears as creamy white patches, often on the tongue or cheeks. It’s more common in people with weakened immune systems, those on antibiotics, or denture wearers.
- Autoimmune and Nutritional Factors: Vitamin deficiencies (especially B12, folate, and iron) or conditions like Crohn’s disease, lupus, or Behçet’s disease can trigger recurring or chronic ulcers.
Treatment Options:
- Topical Pain Relief: Gels and creams containing benzocaine or lidocaine temporarily numb the area. Over-the-counter options like Orajel or Anbesol are commonly used.
- Saltwater or Baking Soda Rinses: These natural rinses help neutralize acids, reduce bacteria, and promote healing. They’re invaluable for mild canker sores or irritation.
- Antiviral/Antifungal Medications: To treat cold sores or oral thrush, a doctor or dentist may prescribe medications like acyclovir (an antiviral) or nystatin (an antifungal).
- Denture Adjustment or Orthodontic Refinement: If appliances are causing sores, your dentist can adjust the fit or shape to reduce irritation and prevent recurrence.
- Nutritional Support: Blood tests can identify deficiencies, and targeted supplements or dietary changes may resolve recurring ulcers linked to poor nutrition.

9. Dry Mouth
Ever wake up with that cotton-mouth feeling that won’t go away? Dry mouth, or xerostomia, is more than just a thirst issue — it can seriously compromise oral health. Saliva helps wash away bacteria, neutralize acids, and prevent decay. When your mouth is constantly dry, those protective benefits disappear. It’s not only uncomfortable — it also puts your teeth and gums at risk for faster deterioration.
Causes:
- Medications: One of the most common culprits, especially in older adults. Many medications — including antihistamines (for allergies), antidepressants, muscle relaxants, and blood pressure meds — can reduce saliva production. Since these are often taken daily, the effect on moisture levels in your mouth can be long-term and progressive.
- Medical Conditions: Diseases such as Sjögren’s syndrome (an autoimmune disorder affecting moisture-producing glands), diabetes, HIV/AIDS, and Alzheimer’s can impair the salivary glands. Dry mouth in these cases is often chronic and may worsen without proper management.
- Cancer Treatment (Radiation & Chemotherapy): Radiation therapy targeting the head or neck can damage salivary glands. Chemotherapy can change the nature and amount of saliva produced, sometimes permanently, depending on dosage and duration.
- Nerve Damage: Any trauma or surgery to the head and neck area — even if unrelated to the mouth — can damage nerves involved in salivary control. This can make the mouth feel dry even if the glands are working normally.
- Dehydration and Lifestyle Factors: Not drinking enough fluids, high caffeine or alcohol consumption, or frequent mouth breathing (especially at night) can all lead to temporary dry mouth. Smoking and chewing tobacco make it worse by drying out the tissues and reducing blood flow to salivary glands.
Treatment Options:
- Stay Consistently Hydrated: Sip water throughout the day — not just during meals. Keep a bottle handy and drink regularly, especially if you’re on medications that cause dryness.
- Stimulate Natural Saliva Production: Chewing sugar-free gum or sucking on sugar-free lozenges encourages saliva flow. Look for products with xylitol, which also helps prevent cavities.
- Avoid Drying Substances: Cut back on caffeine, alcohol, and salty foods. Avoid smoking and using recreational drugs, all of which can drastically reduce saliva flow.
- Use Saliva Substitutes: Over-the-counter saliva substitutes (sprays, gels, rinses) can mimic natural moisture and provide relief, especially overnight.
- Consider Prescription Medications: Drugs like pilocarpine (Salagen) or cevimeline (Evoxac) can stimulate saliva production, but they require a prescription and are typically used for moderate to severe cases.
- Mouth Moisturizing Routines: Use a humidifier at night to combat dryness, and consider switching to toothpaste and mouthwash specifically designed for dry mouth — these are often alcohol-free and contain soothing ingredients.
- Regular Dental Monitoring: Because dry mouth increases the risk of tooth decay and gum disease, you should see your dentist more frequently for cleanings and checkups — often every 3–4 months instead of the standard 6.

10. Toothache or Pain
A toothache is your body’s alarm system saying: something’s wrong. Dental pain should be taken seriously, whether it’s sharp and sudden or dull and constant. Tooth pain can stem from cavities, cracks, infections, grinding, or even referred pain from your sinuses. And the longer you wait to get it checked out, the more complicated (and costly) the fix might be.
Causes:
- Cavities (Tooth Decay): This is the most common cause of toothache. Bacteria in the mouth feed on sugars and produce acid, which slowly eats through enamel. Pain sets in once the decay reaches the inner layers of the tooth (dentin and pulp). This can feel like a dull ache initially, but it may escalate to sharp, shooting pain as the decay deepens.
- Dental Abscess (Infection): When a cavity is left untreated, bacteria can reach the pulp and create an infection. An abscess is a pocket of pus at the root of the tooth and causes intense, throbbing pain, swelling, bad breath, and often a fever. This is a serious condition that needs urgent dental care.
- Cracked or Fractured Tooth: Sometimes, a tooth can crack due to biting hard objects, trauma, or long-term grinding. Even hairline fractures can expose nerves and cause sharp pain during chewing, brushing, or when exposed to hot/cold temperatures.
- Receding Gums and Exposed Roots: As gums pull away from the teeth, they expose sensitive areas of the roots. These roots aren’t protected by enamel, making them prone to pain, especially when eating or drinking hot, cold, or sweet substances.
- Bruxism (Teeth Grinding): Habitual clenching or grinding — often during sleep — puts extreme pressure on the teeth. Over time, this leads to enamel wear, small fractures, and generalized tooth pain or jaw discomfort.
- Sinus Infection: Believe it or not, tooth pain — especially in the upper molars — can be caused by a sinus infection. Because the roots of these teeth are close to the sinus cavities, inflammation or pressure in the sinuses can trigger referred pain that feels like a dental issue.
Treatment Options:
- Accurate Dental Diagnosis: Since pain can stem from a variety of sources, your dentist will likely start with an exam and possibly an X-ray to pinpoint the exact cause.
- Fillings or Restorations: If a cavity causes the pain, a simple filling might be all that’s needed. An inlay, onlay, or crown might be used to restore the tooth’s shape and function for larger decay.
- Root Canal Therapy: A root canal is the go-to treatment for cases involving pulp damage or abscesses. It removes the infected tissue from inside the tooth and seals it to prevent reinfection.
- Tooth Extraction: Severely decayed or infected teeth that can’t be saved may need to be pulled. This prevents the infection from spreading and relieves pain.
- Antibiotics (for Infection): If there’s an abscess or spreading infection, your dentist may prescribe antibiotics to control the bacteria before or after treatment.
- Pain Relief Measures: Over-the-counter painkillers like ibuprofen or acetaminophen can help manage pain in the short term. Cold compresses applied to the outside of the cheek can reduce swelling and numb the pain naturally.
- Treating Bruxism: If grinding is the issue, your dentist may recommend a night guard. In severe cases, bite adjustments or orthodontics may be needed to correct jaw alignment.
- Sinus Treatment (if non-dental): If sinus pressure is the root cause, nasal decongestants, steam inhalation, or antibiotics (if bacterial) may relieve the pressure and stop the referred tooth pain.
Quick Takeaways: Spotting the Red Flags
- Bad breath that doesn’t go away is often a sign of bacteria buildup, dry mouth, or underlying health issues, not just something you ate.
- Bleeding gums, especially when brushing or flossing, usually indicate the early stages of gum disease and shouldn’t be ignored.
- Tooth sensitivity can mean your enamel is eroding or your gums are receding, both of which expose nerve-rich areas of your teeth.
- Visible plaque or tartar isn’t just unsightly — it’s a sign of bacteria buildup that can lead to gum disease, decay, and tooth loss.
- Tooth discoloration may come from foods, drinks, or smoking, but also from poor hygiene, enamel loss, or internal damage.
- Gum recession exposes tooth roots, leading to sensitivity and increased risk of infection, often signaling advanced gum disease or overly aggressive brushing.
- Loose or shifting teeth are major red flags for bone loss and periodontal disease, and often indicate a need for urgent dental care.
- Frequent mouth sores might be caused by irritation, but recurring ulcers or white patches can also point to infection or vitamin deficiencies.
- Dry mouth reduces your mouth’s natural defenses against decay and infection — and is often linked to medications, dehydration, or illness.
- Toothaches, whether dull or sharp, almost always mean something’s wrong — from cavities to infections to jaw issues — and deserve prompt attention.
Listen to What Your Mouth Is Telling You
Your mouth is like a built-in warning system — and when something’s off, it rarely stays silent. From bleeding gums to lingering bad breath, every one of the signs we’ve covered is your body’s way of saying, “Hey, pay attention!”
Poor dental hygiene doesn’t just lead to cavities and yellow teeth. It can progress into serious problems like gum disease, infections, tooth loss, and even affect your overall health. The good news? Most of these issues are totally preventable with consistent care, a good hygiene routine, and regular dental checkups.
If you’ve noticed any of these signs in your own mouth — even just one or two — don’t ignore them. Small symptoms often snowball into major problems when left untreated. Whether you’re 15 or 65, taking action now can save you time, money, and a lot of pain down the road.
So, grab that toothbrush (gently), floss like you mean it, schedule that overdue cleaning, and start giving your oral health the attention it deserves. A healthy mouth is more than just a great smile — it’s a key part of your overall well-being.
Yes, white spots can indicate early stages of enamel demineralization — a sign that cavities may be forming due to plaque buildup and poor brushing habits.
Red, swollen, or glossy-looking gums are early signs of inflammation, often due to poor plaque removal. This may be gingivitis, the first stage of gum disease.
No — if your gums feel sore, it could be due to inflammation or trauma from plaque, or you’re using improper technique (too hard or aggressive).
That slimy feeling is often from overnight bacterial growth due to dry mouth or insufficient nighttime brushing. It’s a sign that your nighttime routine might need a boost.
That “fuzzy” sensation usually means plaque wasn’t fully removed, often because of rushed or inconsistent brushing technique.
Yes. These could be tartar buildup or decay starting below the gumline — both indicators of poor hygiene and early gum disease.
References
- Mayo Clinic. (2022). Bad breath (halitosis): Symptoms & causes.
https://www.mayoclinic.org/diseases-conditions/bad-breath/symptoms-causes/syc-20350922 - American Dental Association (ADA). (n.d.). Gum disease.
https://www.mouthhealthy.org/all-topics-a-z/gum-disease - Cleveland Clinic. (2023). Toothache: Symptoms, causes, and treatment.
https://my.clevelandclinic.org/health/diseases/10957-toothache - National Institute of Dental and Craniofacial Research (NIDCR). (2022). Dry Mouth (Xerostomia).
https://www.nidcr.nih.gov/health-info/dry-mouth - Healthline. (2022). 11 warning signs of poor oral hygiene.
https://www.healthline.com/health/dental-oral-health-warning-signs - Colgate Oral Care Center. (n.d.). How poor dental care can affect your overall health.
https://www.colgate.com/en-us/oral-health/gum-disease/how-poor-dental-care-can-affect-your-overall-health - Hopkins Medicine. (2021). Dry Mouth Remedies: 14 to Try.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/dry-mouth-remedies-14-to-try - WebMD. (2023). Toothaches: Causes, treatments, and home remedies.
https://www.webmd.com/oral-health/guide/toothaches - Penn Dental Medicine. (2022). When is a toothache an emergency?
https://penndentalmedicine.org/blog/toothache - Canadian Dental Hygienists Association (CDHA). (2022). Xerostomia Fact Sheet.
https://cdho.org/factsheets/xerostomia
Check us out on Facebook and Twitter for daily information about Oral Health from Martindale Dental, or visit our offices in Hamilton and St. Catharines.
Have more questions?
Please contact us for all inquiries or to book an appointment with one of our convenient clinic locations. We look forward to hearing from you.




